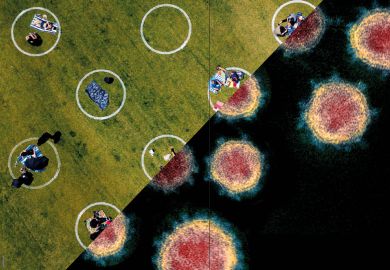
Australia’s energetic Covid research response has been blighted by waste, with clinical trials undermined by parochialism, poor coordination, privacy constraints and skewed priorities.
A review of Covid trials launched in Australia last year has found that many were “underpowered”, enlisting too few participants to generate meaningful results and failing to compensate by recruiting overseas or sharing data.
The findings, published by a University of Sydney team in the Medical Journal of Australia, echo concerns that researchers have ignored sociological aspects of the coronavirus crisis in a rush to unpack Covid’s biological secrets. Experts say that human and government behaviour, which can be far less predictable than the virus, has been implicated in some of the crisis’ most disastrous developments.
In a rush to identify treatments and vaccines, most research groups overlooked people particularly endangered by coronavirus because of illnesses such as cancer, heart conditions or kidney disease, the study found. No trials explored key issues such as public health communication, prevention of community transmission or treatment of “long Covid”.
But a surprising number prioritised interventions that were “not particularly promising”. Six simultaneous trials investigated Donald Trump’s favoured treatment, the malaria drug hydroxychloroquine, potentially putting patients “unnecessarily at risk”.
While the Covid-induced research scale-up was “impressive” for its sheer speed and the “broad array” of drugs analysed, the study reports concerns about “ethical and scientific rigour” and a lack of strategic collaboration.
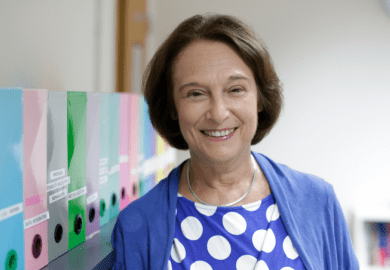
Study leader Anna Lene Seidler, a biostatistician at Sydney, said 80 per cent of the trials had included no plans to share data. None had published the full protocols that would have enabled outsiders to analyse the data, in any case. “We need protocols to fast-track procedures in emergency scenarios that balance both rigour and urgency,” she said.
The Sydney team analysed studies listed between January and mid-November on the Australian New Zealand Clinical Trials Registry, finding 56 Covid-19 trials involving almost 34,000 participants.
Almost two-thirds investigated treatments, mostly drugs, with another 19 looking at preventions such as vaccines. Just two examined diagnosis and education.
Only two trials involved people at “high risk” of poor outcomes, while just 10 had overseas participants. More than four in five recruited exclusively in Australia, obtaining median samples of 150 patients and healthy volunteers – perhaps one-thirtieth of the sample sizes required.
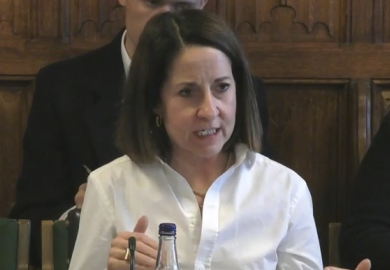
The low Covid caseloads in Australia meant that individual trials were never likely to obtain the sample sizes needed to detect differences in “clinically important outcomes”, the paper says. “It would have been better if researchers had worked together and combined their expertise and resources to conduct larger trials, or a suite of similar trials for which results could be combined upon completion,” said co-author Angela Webster.
The team said that the research community needed to learn from the Covid experience by “creating infrastructure and funding for rapid collaboration, advanced adaptive methodologies and data sharing”.
“In future, with adequate funding for technological innovation, clinical trial registries may play a key role in automatically connecting similar trials and facilitating collaboration.”
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Subscribe
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber?