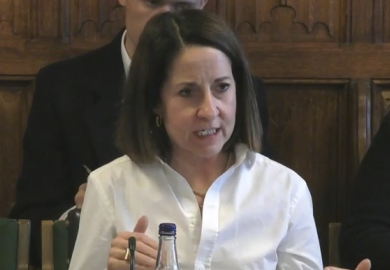
The new director of the US National Institutes of Health, Monica Bertagnolli, is promising that her leadership of the world’s largest funder of medical research will bring much greater emphasis on diversity in clinical trials.
Dr Bertagnolli, nearly a month into office heading the $47 billion (£38 billion) federal agency, held an introductory briefing at which she repeatedly cited the ongoing lack of diversity in trials as a loss for both social equity and overall quality of medical care.
“Our trials can’t just have people who live in large cities, have flexible schedules and are financially well off, with great insurance,” said Dr Bertagnolli, a former professor of surgery at Harvard University and former director of the NIH’s largest division, the National Cancer Institute.
Outside experts said the pledge, if fulfilled, could mean a much-needed overhaul for health-related research, including important adjustments for training at US universities and their medical schools.
Clyde Yancy, a professor of cardiology at Northwestern University and its medical school’s vice-dean for diversity and inclusion, suggested the potential for transformation worthy of comparison to Dr Bertagnolli’s long-serving predecessor, Francis Collins, and the foundational changes he represented as leader of the Human Genome Project.
The need for meaningful diversity in the populations of study participants was especially critical now, Professor Yancy said, because the rapid rise of personalised medicine and genomic-based treatments raises the risk of extremely costly mistakes if solutions are based on only small segments of the nation’s overall population.
“We have this opportunity, now with a new director, to really leverage the success we had bringing genomics along because of Francis’ leadership, and to have Dr Bertagnolli say this is another platform that we intend to operationalise,” Professor Yancy said.
The areas of necessary change include some standard practices at US medical schools, said another expert, Jonathan Jackson, an assistant professor of neurology at Harvard and executive director of the Community Access, Recruitment, and Engagement Research Centre at Massachusetts General Hospital.
Currently, Dr Jackson said, medical trial design puts a heavy if unspoken value on maximising speed and reducing costs. It’s almost cliché, he noted, for a practice trial in academia to involve rounding up a few undergraduates willing to test an intervention. “The idea is to try to just collect people whenever they’re convenient,” he said. “And what you find is that these principles are conveyed to you in a way that is not usually explicit, but is certainly implied in terms of trying to rush people to get a paper out.”
The world just got another taste of the risk of that mindset persisting into the professional sphere, Professor Yancy said, when the drug company Novo Nordisk announced the results of a medical trial involving more than 17,000 participants from 41 countries showing that the antidiabetic drug semaglutide offers a major reduction in the risk of cardiac events. But for those looking closely at the data, he said, it became clear that only 23 per cent of the study participants were women and only 4 per cent were black.
That immediately raises the question of whether the benefits of semaglutide will apply to everyone, Professor Yancy said. “And we have some tentativeness about that answer,” he said.
Dr Bertagnolli, who was raised in rural Wyoming, said her vision of diversity includes geographic differences as well as those of race, gender and wealth. She credited the NIH with important progress but said it needed more, including finding ways that the agency – which works most directly with the research community – can engage more directly in the nation’s overall healthcare system.
She also noted that the cancer institute, under her leadership, had research networks that were enrolling between 30 per cent and 40 per cent of under-represented groups in their clinical trials. “It’s complex and it’s challenging, but I think we’re making great progress,” she said.
Dr Bertagnolli does, however, take office at a time – following the Covid pandemic and the departure of Dr Collins, renowned for his ability to charm lawmakers on both sides of the political divide – when the NIH is facing a tougher budgetary environment. The Democrat-controlled US Senate has proposed a 2 per cent budget increase for the NIH while the Republican-led House of Representatives has voted for a 6 per cent cut.
Reworking clinical trial operations to include more people from rural and other difficult-to-reach communities could add even more costs to NIH grants, Dr Jackson said. But the added costs would be marginal compared with the billions of dollars that the NIH already spends on medical trials, and well worth the expense if it makes results more reliable, he said.
And the extra cost might be a lot less than expected, Professor Yancy said, because the NIH could help researchers develop more effective ways of reaching remote populations, such as sending test kits sent through the post, and making greater use of partner facilities and medical clinics far from major medical centres.
Some barriers to enrolling more diverse populations in clinical trials were largely a matter of better training, said Monica Baskin, a professor of medicine at the University of Pittsburgh and associate director of health equity at its Hillman Cancer Center. Some trial protocols, for instance, impose overly broad terms of exclusion that do not really serve a medical necessity, Professor Baskin said. And some doctors simply do not suggest trial participation to certain patients, for reasons that include inaccurate assumptions that they are not interested, perhaps because of race-based medical abuses that happened in past generations, she said.
“It’s definitely a really critical problem,” she said. “And, certainly, NIH is in a position to reinforce the value of that representation in terms of its funding and requiring that for all of its clinical trials.”
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Subscribe
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber?