The mantra of excellence is ubiquitous in the research funding system of the UK and other scientifically advanced nations. When money is limited and international competition for prestige is fierce, surely it makes sense to concentrate spending on the projects most likely to make a big scientific impact?
As Lord Willetts, then minister for universities and science, put it in 2010: “Excellence is and must remain the driver of funding decisions, and it is only by funding excellent research that the maximum benefits will be secured for the nation.”
Yet this is to look at the funding system entirely from the researchers’ perspective. It is excellence for science, not for society.
UK Research and Innovation is pledged to ensure that “everyone in society benefits from world-leading research and innovation”, while the National Institute for Health Research’s mission is to “improve the health and wealth of the nation”. However, these goals are not being achieved.
Data on the cost of illness have been available since the 1950s, and the World Health Organisation has been producing research on the burden of disease since 1990. This combines early death and disability caused by different diseases into one measure, the “disability-adjusted life year”.
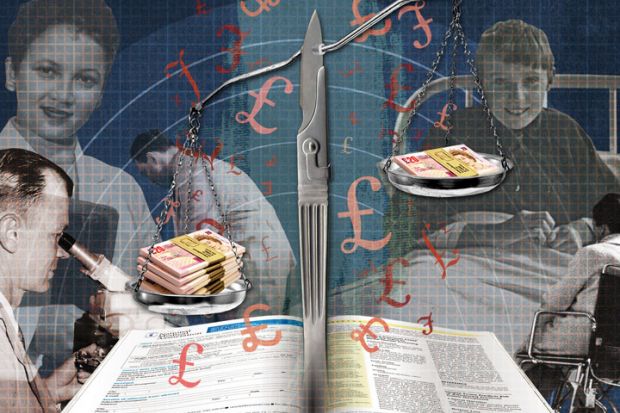
A few years later, the National Institute for Health and Care Excellence (NICE) began ratifying treatments for the NHS provided that they cost between £20,000 and £30,000 per year of improved life, measured as a “quality-adjusted life year”. This created an exchange rate for health economists to determine the human and financial cost of each illness, giving funders a mechanism to target equitable amounts of funding for each illness. But they ignored it.
This is no longer tenable. Four months after Willetts’ statement, the Public Sector Equality Duty was signed into law. At this point, all UK medical research funding – if it wasn’t already – probably became unlawful. This is a bold statement, but consider the Equality and Human Rights Commission’s observation that “the Court of Appeal has made it clear that public bodies should place considerations of equality, where they arise, at the centre of formulation of policy, side by side with all other pressing circumstances of whatever magnitude”.
Moreover, “a body subject to the duty will need to be able to show that it had adequate evidence to enable it to have due regard” to that duty. Yet neither NIHR nor UKRI can break down their spending by the characteristics protected by the Equality Act – which, as well as disability, include age, sex, race and gender orientation.
Looking at disability, deafness receives only 25 per cent of the funding that it should relative to its impact on society, according to the WHO data. It is the worst-funded health cause on this basis – and the fact that this hasn’t changed in the past five years suggests that funders are unconcerned.
This is no longer a conceptual argument. After a legal challenge by the Equality and Human Rights Commission Scotland, the Chief Scientist Office, NHS Scotland’s research funder, has agreed to conduct an “equality impact assessment” into its funding.
However, this doesn’t mean that funders will embrace change. When I made the same challenge to UKRI, the body’s chief executive, Sir Mark Walport, said that equality consideration did not form part of UKRI’s “agreed governance framework”.
As well as inequalities across major illness categories, there are inequalities within them. Between 2011 and 2016, for instance, the Medical Research Council spent five times more on schizophrenia research than on anxiety, despite anxiety’s having more than twice the disease burden and a higher economic cost. This discrepancy also disadvantages women, who are relatively more affected by anxiety. Minority groups, such as the BME or LGBT communities who are more affected by mental illness, are also being disadvantaged because in a general research project they are unlikely to form statistically significant groups.
Funding purely on the basis of excellence ensures that underfunded conditions stay in a poverty trap of low capacity and low success rates. And it doesn’t make much sense on its own terms. Its advocates warn that abandoning excellence would result in the wasting of scarce funding on mediocre research. Yet in the 2014 research excellence framework, the average scores for the psychology, psychiatry and neuroscience subpanel are within 3 per cent of the mean for all five biomedical units of assessment.
This constitutes reasonable evidence that historically underfunded mental health research is not mediocre relative to other areas of UK medical research. The issue is that there are not enough academics to generate the research needed to match the impact of mental health on society. Until recently, funders have not attempted to increase capacity, as the Equality Act would oblige them to.
As for prospective returns on investment, if our funders were really able to assess that accurately, surely their staff would be in the Caribbean by now, on the back of large biomedical investments?
The UK’s researchers are no doubt excellent. Isn’t it time that our funders were, too?
Alex Conway is chief executive officer of Miricyl, a children’s mental health charity based in Edinburgh.
POSTSCRIPT:
Print headline: Health research funders should take account of potential impact
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Subscribe
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber? Login