How can we better monitor TB cases among our children?
Sponsored by

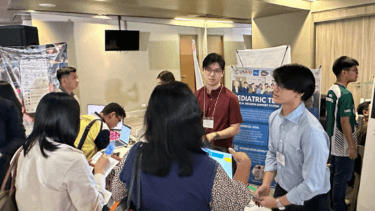
A project led by De La Salle University’s IT faculty sought to develop a system that collects data on TB cases among Filipino children. Funded by USAID through URC, it is envisioned to support medical professionals as well as local government units across the country toward the effective management of the disease.
She shares that the project was conceived during her discussions with Dr. Elmer Soriano of CIVIKA and Mr. Virgilio Linis on how they could help manage records of TB health cases. While pursuing her master’s degree at DLSU, she was exploring a health-related topic and Open Data.
In the course of her research, she has noted that TB has remained one of the deadliest diseases in the country. “Children are the most prone to having lifelong threatening effects of tubercolosis” Ching points out.
For the Clinical Decision Support System through rule-based algorithm, the research team used the Department of Health’s existing Guidelines for the National Tuberculosis Control Program Manual of Procedures, which provides the basis for assessing a patient’s symptoms. If a person shows all four of the cardinal symptoms, that person will be presumed to have TB.
With the system, it will be more efficient to collect and generate data across the archipelago. “In the local setup, since we have several islands, not all have the healthcare facilities or physicians available, especially in far-flung areas,” she notes.
“So, even with the TB dots, even with the free medicines available, if you cannot detect it, you cannot treat it. And it’s easily spreadable because it’s an airborne disease. Actually, before I studied tuberculosis, I did not know that it’s that serious,” she shares.
With the collective data, the system can determine probable areas affected by tuberculosis. The team has made test runs in the areas of General Trias, DLS-MHSI, and Trece Martires in Region IV-A using a rule-based algorithm decision tree system. This system is based on different combinations of data, such as the symptoms of the patient, lab results, and medical history, to name a few. The team has already generated over 11,000 combinations.
According to Ching, the system can be implemented with encoders who do not need to be medical professionals. It is envisioned to be deployed in healthcare facilities like barangay health centers, where midwives and volunteers are tapped when doctors are not available.
The pediatric TB clinical decision support system simplifies diagnosis for presumptive, active, and latent pediatric TB patients with its user-friendly interface and one-click diagnosis feature. It analyzes patient records, follows Department of Health guidelines, and incorporates physicians’ practices for accurate diagnoses.
Initial iterations of the clinical decision support system showed promising improvements in diagnosis accuracy and treatment recommendations. User feedback during testing informed enhancements, leading to a streamlined Version 4.0 with a more intuitive interface for healthcare providers, marking ongoing progress in refining the system for better TB diagnosis and treatment decisions.
Looking forward to the next phase of the project, Ching shares that DOH has expressed support for introducing the software at a wider scale, covering the whole of Region IV-A.
“Technology is rather not a replacement, but a tool or an aid that can help healthcare professionals clinically diagnose patients effectively,” Ching says. “A single expert can only do as much. But when we combine all of our expertise, we can create a great impact.”
Contact: Dr. Michelle Renee Ching | michelle.ching@dlsu.edu.ph