New invention can improve the assisted reproduction success rate
Globally, as many as 10 per cent of couples cannot have children naturally. 33 per cent of assisted reproduction cycles are successful – a healthy baby is born. To help couples have children, KTU researchers and their partners are working on a diagnostic system to determine whether the uterus is ready to accept an embryo grown in a petri dish.
Vidas Raudonis, professor of the Faculty of Electrical and Electronic Engineering (EEF) of KTU in Lithuania, and an expert in the field of artificial intelligence (AI), speaks about the invention of Kaunas University of Technology (KTU), Lithuania and partners.

The project partners are Dts Solutions, the Reproductive Medicine Centre (RMC) of Kaunas Clinics at the Lithuanian University of Health Sciences (LSMU) and the Competence Centre on Health Technologies, Tartu, Estonia (CCHT).
Aims to help couples have children
Prof. Raudonis says that the technology developed by him and his partners is a medical diagnostic solution to determine whether the uterus or, more specifically, the endometrium, the inner layer of its tissues, is ready to receive a human embryo grown in a petri dish.
“As many as 10 per cent of the couples cannot have children naturally, and only 33 per cent of assisted reproduction cycles are successful, resulting in a healthy baby. Together with our partners, we want to help couples to have children, which is why we are developing a diagnostic system that focuses on personalised medicine,” says Raudonis.
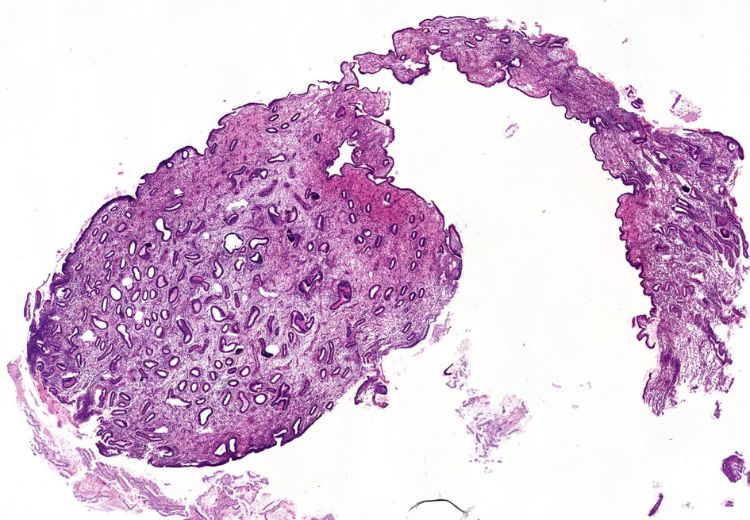
The KTU researcher explains that based on contemporary computer vision algorithms, the diagnostic system decides the uterus’s receptivity by analysing the endometrial layer’s histological image. He adds that the histological images are zoomed-in digital images of thin layers of tissue, obtained with a digital microscope.
According to Raudonis, just like a pathologist, the AI model implemented in the algorithm pays attention to the tissue cells, their size, location, endometrial glands, epithelium and other visually noticeable details, and forms a numerical answer based on them. This is often interpreted as a probability between 0 and 100 per cent of the uterus’s readability to accept the embryo.
The AI-based system provides cheaper, safer and more efficient diagnostics
“This diagnostic system is needed when a woman is unable to conceive through repeated assisted reproduction procedures. In this case, more complex procedures are carried out, which aim not only to have a high-quality and healthy early-stage embryo but also to determine the exact implantation window during which the uterus is fully ready to receive the embryo,” says Prof. Raudonis.
He notes that, until now, receptivity has been determined by DNA testing from a biopsy of the inner layer of the uterus. However, not all assisted reproduction clinics can carry out such tests in-house, and often the transport of the biopsy sample is complicated, as it is necessary to ensure that the DNA is not degraded during transport.
“Meanwhile, our system can be accessed on our website. Just upload a digital image of the tissue and the diagnosis of receptivity will arrive in a few seconds. This saves time, money and women’s health,” explains Raudonis, Lead Researcher at Smart Automatic Control Systems and Robotics research group.
He says that the system analyses histological images and decides based on the visual features, so no sophisticated equipment is needed to diagnose. It only requires a digital microscope that can take a very close-up picture of the biopsy sample.
Almost 90 per cent accuracy in distinguishing receptivity levels
The KTU professor explains that the AI methods were used to automatically find visual clues to distinguish between different stages of endometrial receptivity. Raudonis says that he and the scientists from the Reproductive Medicine Centre (RMC) of Kaunas Clinics at the Lithuanian University of Health Sciences developed a statistically significant database and used it to train the AI models.
“To date, we have found that AI models focus mostly on areas where endometrial glands are visible. This is also where pathologists see the differences between the different stages,” explains an artificial intelligence expert, and KTU researcher.
He explains that AI approaches are akin to a black box, with decisions not fully explained. Nevertheless, the researchers can already glimpse inside this box to find out on which areas of the digital image the AI focuses most in the decision-making process.
“We noticed that the focus map of the AI model shows more clearly the areas where the margins of the endometrial glands, the central part of the glands and the stroma close to the epithelium are located. We believe that the appearance of these zones determines the AI model’s decision. Currently, with the available database for testing, we can achieve 89 per cent accuracy in distinguishing the three stages of receptivity,” says Raudonis.
He explains that the receptivity of the endometrial layer is a series of transitional stages of the uterus: “These stages can be divided into pre-receptive, receptive and post-receptive. Naturally, they can be calculated by observing the menstrual cycle. However, if the cycle is disturbed or if hormones are used to stimulate the uterus, the receptive stage is not as straightforward to calculate.”
The invention is ready to be tested in real-life
This requires a closer look at the inner uterine tissue itself, the genes or the morphology of the cells in the tissue, otherwise known as the visual signs. It is the histological images, he says, that encode the information needed to make a diagnostic decision.
“Histological images show zoomed-in views of the cells in the uterine tissue layer, their nuclei. The size and location of the cells and glands are the first direct signs that the uterus is ready to receive an embryo,” says the KTU researcher.
The invention has reached the fourth technological readiness level (TPL4), which means that the algorithms are almost at the stage where they should be tested in real life. The AI models, says Raudonis, are continuously being tested using data from real medical practices.
“In my opinion, the outlook for this invention is very positive. If the proposed diagnostic system is trusted by the medical sector, we will probably see more healthy babies,” says the KTU professor.
According to Raudonis, Dts Solutions is the main executer of the international project, which is being carried out by the RMC of LSMU Kaunas Clinic and the Competence Centre on Health Technologies, Tartu, Estonia (CCHT). Dts Solutions is an IT company, which is working to make the technology available to the whole assisted reproduction market. Meanwhile, the health sciences partners are taking care of the data and data management.
“The energy and efforts of Dr Linas Eidimtas of Dts Solutions have brought us all together. Prof. Eglė Drejerienė, Dr Agnė Kozlovskaja-Gumbrienė of RMC at LSMU Kaunas Clinics suggested the idea of contacting the Estonian partners. Prof. Andres Samulets of the Estonian CCHT has made a great effort in the field of receptivity,” says Raudonis, KTU professor working in the field of artificial intelligence solutions.
Learn more about artificial intelligence research at Kaunas University of Technology, Lithuania.