Learning translational medicine can make doctors more effective
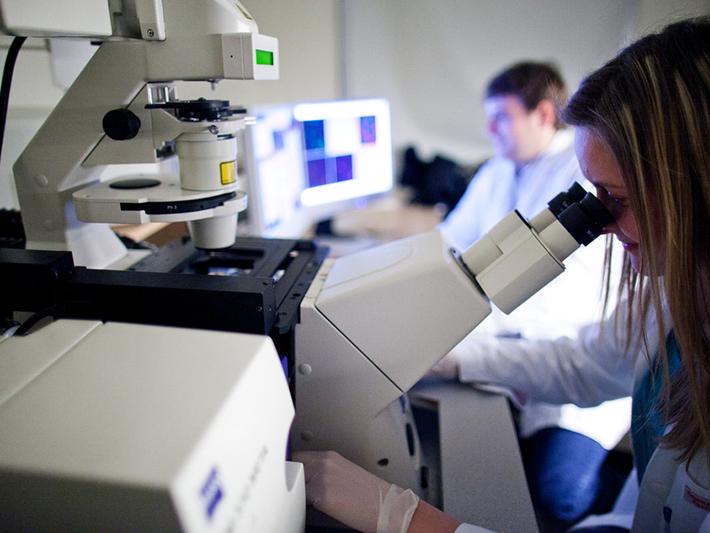
Data used to be collected in the laboratory. Researchers would ask patients to fill out questionnaires or they would conduct clinical research. PhD theses were typically based on this kind of research. Unfortunately, in many cases, researchers were often less concerned about whether their research was beneficial to society than if it was easy to carry out.
Today, information technology and data have changed how research is practised. I believe postgraduate education at universities should equip students with knowledge that can be used for the benefit of society in everyday life.
What has also changed is that scientific results are produced much more quickly than ever before. Scientific activity has increased 25-fold since 1950. In 2000, a year would see 500,000 studies published compared with 2 million today. An enormous amount of data is available, but analysing it is not the big challenge. What is really important is that researchers ask the right questions.
- How practical education and talent management support medical students
- A case study in developing the next STEM generation
- How to promote primary interest in basic medical education at the undergraduate level
In modern postgraduate training, it is necessary to ask questions that are directly related to society or to a particular disease. Then, the available data should be examined to find out what answers can be obtained from them. This is what translational medicine, which includes all scientific activities that can directly benefit patients, helps us to do.
Beneficial for students, society and universities
Acquiring knowledge of translational medicine is beneficial not only for students, who gain tools that can be used in their everyday work, but also for society, as diseases can be treated more effectively. It is also good for universities because the research conducted by PhD students improves their scientific outcome.
So far, only PhD students have been able to participate in translational medicine training at Semmelweis University. In the past three years, more than 260 from 21 countries have entered our programme, mostly from patient care. From the next semester, we will launch a one-year MSc course, which will have the same four pillars as the PhD training. The first pillar is clinical methodologies, which help students to access the latest scientific results. The second is biostatistics, which helps them understand results and decide how reliable they are. The third pillar includes soft skills such as time management, smart communication and crisis management. The students’ own projects are the fourth pillar. These four pillars make translational medicine training unique.
Screening protocols for cystic fibrosis-related diabetes
The students participating in our training programme already have outstanding results. For example, we have PhD students researching cystic fibrosis at the Heim Pál National Pediatric Institute in Budapest. This congenital genetic disorder increases the risk of diabetes, which is typically discovered late, when complications such as deteriorating vision arise.
However, if diabetes were detected earlier, before the onset of symptoms, treatment could be started before organ damage occurs. This is the reason why this hospital started screening children with cystic fibrosis for diabetes between the ages of three and four.
The current guidelines only recommend diabetes screening at the age of 10, but research shows that this recommendation needs to be revised and updated. With earlier screening, diabetes can be detected in 30 per cent of children many years before symptoms appear. This could prevent complications of untreated diabetes.
Finding the best surgical solution for cholesteatoma
At the Bajcsy-Zsilinszky Hospital in Budapest, otolaryngologists have launched research on cholesteatoma, a benign tumour of the middle ear that can only be treated by surgery. The background of this research was that doctors had observed that, despite surgery, the recurrence rate of this disease was high. They started searching for the best surgical method based on the results of the studies available.
As a result, it was found that one type of surgery is much more effective than the others, and now this method is used for all patients. This has significantly reduced the risk of recurrence. A scientific paper on this achievement has been published in one of the most prestigious journals of otolaryngology. The greatest success of the learning-by-doing method is its speed, which in this case means that the research results could be applied in practice before the researcher has even defended their PhD.
Antibiotic usage in pancreatitis
Previously, a PhD student investigated the use of antibiotics in pancreatitis at the Institute for Translational Medicine at the University of Pécs, and he achieved outstanding results. Even before the scientific paper on the subject was published, it was possible to reduce antibiotic usage in this disease to 40 per cent of cases from the previous 80 per cent.
In the past, doctors used antibiotics much more frequently because they interpreted signs of inflammation as signs of infection, not knowing how to differentiate between the two problems. The methodology for this was highlighted by the PhD student’s research, also before he defended his PhD thesis. This method has since been used in university clinics in Hungary and in the hospital at Székesfehérvár, one of the largest cities in Hungary. Antibiotic usage has been significantly reduced everywhere. These results also show that scientific results with the right methodology can be quickly translated into everyday medical practice, making patient care much more effective.
As our experience with the translational medicine programme is well established, we are happy to share it with other universities and welcome applications from students and supervisors from other institutions.
Péter Hegyi is the deputy chair of clinical and veterinary science section at Academia Europaea, and a professor in the Centre for Translational Medicine at Semmelweis University, Budapest.
If you’d like advice and insight from academics and university staff delivered direct to your inbox each week, sign up for the Campus newsletter.