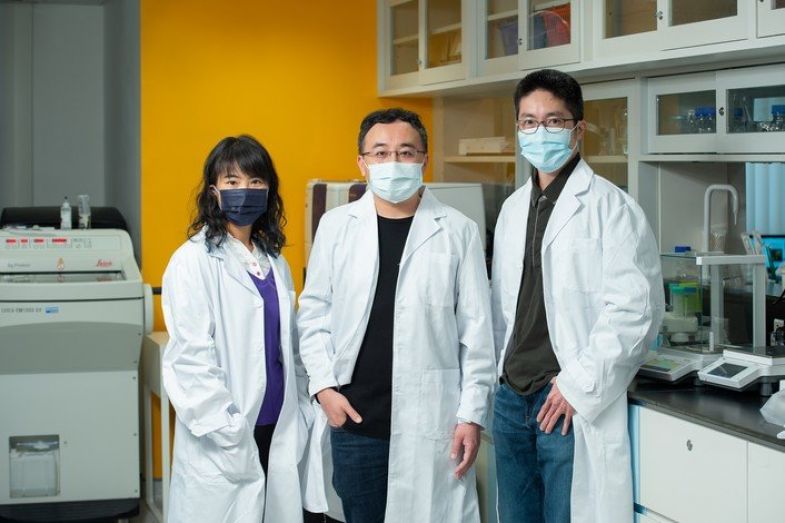
Professor Gary Wong Ka-leung (centre), Dr Lung Hong-lok (right) and Dr Law Ga-lai, an Associate Professor from The Hong Kong Polytechnic University, have developed a novel dual-targeting drug for treating cancers associated with EBV.
A Hong Kong Baptist University-led (HKBU) research team has developed a novel drug that has the potential to become a next-generation treatment for cancers associated with Epstein–Barr virus (EBV).
The peptide-linked drug, which is responsive to the acidic environment found in tumours, is the first known agent to have successfully targeted two viral proteins that are simultaneously produced by EBV. It also offers a new strategy by increasing the uptake of anti-cancer drugs in tumour cells, thus allowing the application of lower drug dosages which helps reduce treatment side effects and health risks. The research results were published in the international academic journal Advanced Science.
EBV is one of the most common viruses in humans, and it has infected more than 90% of the human population worldwide. It is widely known that the virus plays a key role in several cancers such as nasopharyngeal carcinoma (NPC), which is highly prevalent in Hong Kong and southern China.
Led by Professor Gary Wong Ka-leung, Professor and Head of the Department of Chemistry at HKBU, and Dr Lung Hong-lok, Assistant Professor of the Department of Chemistry at HKBU, the research team constructed a novel drug with a peptide, i.e., a component of the building blocks of various proteins, that can target two EBV-specific viral proteins – Latent membrane protein 1 (LMP1) and Epstein–Barr nuclear antigen 1 (EBNA1). They are the viral proteins that are expressed in all EBV-infected tumour cells, and both play a vital role in the development and progression of EBV-associated tumours.
Leveraging the success of the first-generation drugs developed by the research team in recent years, this novel dual-targeting drug employs the treatment mechanisms of: (1) targeting and binding to EBNA1, making it no longer functional, and (2) inhibiting LMP1 and serving as an imaging agent. Since LMP1 is more accessible to drug targeting due to its presence on the surface of cells, the ability of the new drug to selectively identify EBV-infected cancer cells is largely enhanced. In addition, the drug’s excellent sensitivity to the acidic environment found in tumours can minimise its off-target rate and reduce damage to normal cells.
The novel drug was tested in an animal model by injecting it into mice with EBV-positive NPC tumours. The results showed that a low drug dosage of 12.5 mg per kg of body weight could reduce the NPC tumour size by half. In addition, the average body weight of the mice increased slightly during the experimental period, indicating an improvement in their health condition. The study also showed that the drug can emit unique responsive fluorescent signals once it has bound to the viral proteins, illustrating its potential role in tumour cell imaging.
“The experimental results are good indicators that prove the drug’s efficacy and safety. Since this is the first example of simultaneous imaging and inhibition of two EBV viral proteins, it can serve as a blueprint for a next-generation drug for the safe monitoring and treatment of a specific cancer,” said Professor Wong.
















